Some people with a stoma can have stoma reversal surgery, with the aim of restoring normal bowel function. For many people, this results in a successful outcome; however, the operation can sometimes present a new set of challenges.
Facing the question
Around a third of the UK’s roughly 120 000 stomas are classed as temporary. Most of these are loop colostomies or ileostomies, as opposed to end stomas, which are more likely to be permanent (see box).
However, for a minority of people with end stomas, reversal is possible. The procedure is often more complex than for other sotma types, as it involves re-opening the abdominal wound so that the surgeon can locate the two sections of bowel. This is often made difficult by the presence of scar tissue (adhesions) and may result in a temporary stoma for a further few months.
Reversal isn’t for everybody, and being presented with the option can cause a mix of emotions. Some people feel their stoma has saved their life or greatly improved its quality. Others, especially older or frail people, may not want to go under anaesthetic again and risk a further operation. Fortunately, all these considerations can and should be discussed with the surgeon and stoma care nurse. They will offer their expert advice, but the final decision is always yours.
Making sure
Stoma reversal is usually offered 3–6 months after the initial surgery to make the stoma, but this depends on the ostomate’s individual health, treatment and circumstances. The consultant will want to check that the newly joined bowel (anastomosis) has completely healed. These tests may require taking a laxative. If you don’t normally use a drainable bag, you should request one from your stoma nurse before these tests take place, as the output from your stoma may be very watery for a day or so afterwards.
Once the consultant is happy that everything has healed, they will arrange a date for the stoma reversal operation.
Going under
You will usually be admitted to hospital on the day of the operation. Reversals for both loop colostomies and ileostomies are performed in the same way, under general anaesthetic. The operation is not as complex as your previous surgery. An incision will be made around the stoma to enable the surgeon to reconnect the two pieces of bowel, leaving a small wound where the stoma has been. The stitches here will either be dissolvable or will be removed after 7–10 days at your GP surgery or at your hospital follow-up appointment.
Sometimes the surgeon prefers to leave the small wound open so that it can heal (granulate) from the bottom up. This usually takes 2–4 weeks. You may be shown how to dress the area, or you will be referred to your district or practice nurse when you go home.
Loops, ends and barrels
Depending how a stoma is formed, it will be classified as either an end, loop or double-barrelled ostomy.
To form an end stoma, the bowel is cut and one end is pulled through the body wall. The rest of the bowel below the cut is either removed or closed shut inside the body.
In a loop stoma, a loop of intact bowel is pulled through the abdomen. This loop is then surgically divided into two ends: one functional end, which produces the output, and a non-functional end, which may produce some mucus. This makes the two halves easier to reattach in reversal surgery.
A double-barrelled stoma is similar to a loop stoma, except that the two ends are disconnected and pulled through the skin surface at different points.
Early days
When you return to the ward after surgery, you will have a drip in your arm, which will keep you hydrated. You will be given painkillers as required, in order to keep you comfortable. Initially, you will be allowed sips of water, and, if you don’t experience any sickness, this will slowly increase to free fluids. If these are tolerated, you will then progress to a light diet, consisting of foods like soup, jelly and ice cream.
Sometimes the bowel can take a while to start working normally again, and food, gas and liquid may not be moving through the digestive tract properly. This is known as an ileus. If this happens, you will have to stop eating and drinking until it is resolved.
One of the first signs that the bowel is starting to work again will be when you start passing wind from your bottom, although this may take a few days. It can often take 2 or 3 days before you feel the urge to go to the toilet.
Changes to look out for
In the first few weeks after your operation, your bowel pattern can vary enormously. Everyone’s experience is different, and it can be affected by diet, the amount of bowel removed and where the bowel was removed from, as well as any chemotherapy or radiotherapy undertaken before or after surgery.
During this early period, it is common to experience either one or a combination of the following:
• Urgency (need to get to the toilet as soon as possible)
• Incontinence or leakage of stool
• Diarrhoea
• Constipation
• Passing small amounts of stools frequently and not feeling you have completely emptied your bowels
• Difficulty in distinguishing between wind and stool
• Passage of mucus and, occasionally, a little fresh blood into the toilet
• Pain in your bottom after going to the toilet.
All of these are normal and often temporary problems. They will settle over time, although for some people it can take up to a year.
If you are experiencing urgency or leakage of stool, ask your stoma care nurse or physiotherapist about exercises you can do to strengthen your pelvic floor muscles. These muscles will not have been used very much during the time you had your stoma. You may also wish to use a thin pad inside your underwear, especially at night.
What to do if, after stoma reversal, I have...
Constipation
• Eat more fruit and vegetables
• Eat more fibre (wholemeal bread, cereals)
• Drink more fluids (8–10 glasses per day)
• Drink a glass of prune juice in the evening
• Take plenty of gentle exercise (walking is good)
• Watch out for medications that can cause constipation (including painkillers)
• Consider a mild laxative on prescription
Loose stool
• Eat more carbohydrates (white bread, pasta, rice)
• Eat less citrus fruit, spicy food and chocolate and avoid large fatty meals
• Drink less tea, coffee and fizzy drinks, as caffeine is a bowel stimulant
• Avoid products containing sorbitol (an artificial sweetener)
• Watch out for pure fruit juices and some vegetables, which can cause diarrhoea in some
• Watch out for medications that can cause diarrhoea (including antibiotics)
• Consider anti-diarrhoeal medication
Too much wind
• Eat more bio yoghurt (which can reduce wind)
• Eat fewer baked beans and vegetables, such as cauliflower, cabbage, onions and sprouts
• Eat meals at regular intervals (to avoid long periods with an empty stomach)
• Drink less beer and fizzy drinks
• Avoid eating and drinking at the same time
• Avoid chewing gum or smoking
Taking care of your skin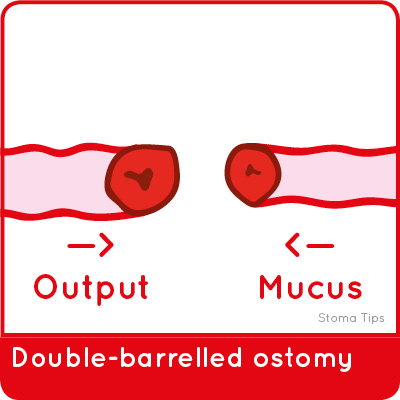
Frequent loose stools and occasional leakage can make your bottom sore. This problem can be reduced by gently wiping your bottom after each bowel action, gently cleaning the area with warm water and patting it dry using a soft cloth. Avoid using disinfectant, salt baths, perfumed soaps or talc. Baby wipes can be used, so long as they don’t contain alcohol. The following tips can also help:
• Apply a thin layer of barrier cream (your stoma nurse can recommend one)
• Irritation can cause itching, but try not to scratch
• Wear cotton underwear and avoid tight trousers and thongs.
Eating right
In the first few weeks following your operation, you may find that you don’t have much of an appetite. This is normal. Initially, it is probably best to eat four or five small, frequent meals or snacks throughout the day, such as sandwiches or biscuits with cheese, until your appetite returns. Eating three large meals can make you feel bloated.
It helps to ensure you chew your food well. If you are experiencing either diarrhoea or constipation, your stoma nurse or dietitian will advise you what to eat and what to avoid. If you are constipated, loose or windy, there are a number of diet and lifestyle adjustments you can make. Medication may be needed if diet alone does not improve your bowel pattern. If you have constipation, you may be prescribed a mild laxative. If you have diarrhoea, you may be prescribed medication to slow down and bulk up your stool.
However, the aim is to return to a healthy, well-balanced diet. To help to repair body tissue, this should be high in protein, such as eggs, fish and lean meat, as well as nuts, beans and certain grains and pulses.
Coming home
It is important that you do not go home until your bowels have opened. Your hospital stay will depend on the extent of bowel disruption and how you are coping with it. This is likely to range from 3–7 days, but it may be longer. When you get home, it is normal to feel tired. However, it is important that you stay active and do gentle exercise, like walking. You should not do any heavy lifting or strenuous exercise for 3–6 weeks.
You should be able to drive when you feel safe enough and comfortable enough to do so. Most people will be able to return to work after 2–6 weeks, as long as their job is not too physically demanding. It may help to go back on a part-time basis at first if possible. If you have any unopened boxes of stoma supplies, your stoma nurse may be able to take these back from you. Alternatively, spare equipment can be given to charitable organisations.
References
• Colostomy UK. Stoma reversal. 2019
Conclusion
Many people who take the option of stoma reversal expect bowel function to return to normal after the operation, but this may be unrealistic and unachievable. Your stoma nurse will be able to offer support and advice, both during your hospital stay and when you get home.
Knowing what to expect and being well-informed can reduce anxiety and contribute to your recovery. Ignorance is not bliss!

 Sue Reed is an independent clinical nurse specialist in stoma care based in London
Sue Reed is an independent clinical nurse specialist in stoma care based in London
The contents of this page are property of MA Healthcare and should not be reused without permission

