Some health problems involving the digestive tract, such as colorectal cancer, may require an operation that results in a temporary stoma (often an ileostomy). The temporary stoma diverts digested waste into a disposable pouch attached to the abdomen. This ’defunctions’ the lower part of the bowel, typically to allow it to rest and heal before it is reversed. This article briefly explains some of the issues to consider before and after going for stoma reversal surgery.
Reversal
Once the lower bowel is able to heal, then it should be possible to undergo a reversal. In a reversal, the temporary stoma is closed, and the two separated ends of the bowel are rejoined (called an anastomosis). This is usually a very welcome event, which will hopefully allow a return to a more conventional way of evacuating bodily waste and may signal successful completion of a long series of treatments.
However, stoma reversal cannot always be predicated or guaranteed. Healing may be faster or slower than expected, and, in some cases, a permanent stoma may turn out to be the most appropriate option.

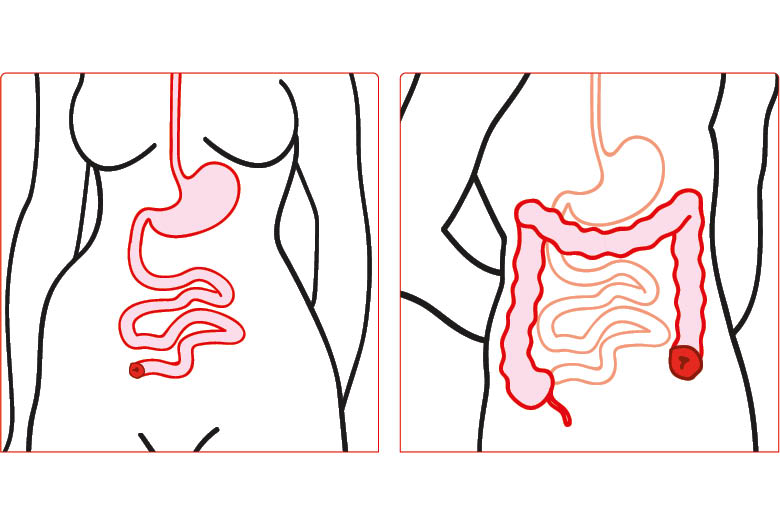
Ileostomy and colostomy
Different functions
If a temporary stoma is successfully reversed, that is not always the end of the story. Operations resulting in stoma formation often involve permanently removing sections of the digestive tract, which can include part or all of the large bowel and/or rectum. A reconnected digestive tract may be very different to how it was before an operation, and so it may also function differently. Some things, such as going to the toilet, may never be quite the same again.
Different people tend to experience different changes. The main potential issues are:
• Clustering: having to go to the toilet several times within an hour
• Constipation: finding it difficult to pass stools
• Frequency: needing to go to the toilet more often than before
• Urgency: feeling the need to rush to the toilet and being unable to wait.
These problems tend to result from changes to the bowel caused by the disease, the operation and the recovery period. This might involve damage to tissue and nerves used to control bowel function. Often, after surgery, the bowel and rectum simply have less capacity to store stool before it is passed, which means going to the toilet more frequently and passing smaller amounts at a time.
These problems often improve with time. Some issues are temporary, such as diarrhoea resulting from the bowel becoming inflamed while it was not being used; in this case, using the bowel again should reduce inflammation. Bowel issues are most likely to improve within the first 3 months after an ileostomy is reversed, and they can continue to get better for up to 2 years.
Decisions, decisions
Healthcare services are increasingly trying to involve people in making decisions about their surgical options. However, these decisions are often difficult, and people need clear and accurate information to make them. When we are told we need an operation that includes stoma formation, it is often difficult to know what to do for the best. For example, there might be misunderstandings of what a stoma is, or how long exactly temporary might mean. Good information can be essential for coping with changes to your body and body image.
It is important to remember that you can choose not to have your stoma reversed at all, and some people find that they are happier with their stoma.
Alternatively, if you do have a stoma reversal and you are badly affected by bowel problems, which other treatment options do not help to your satisfaction, then you can choose for the surgeons to give you a permanent stoma (usually a colostomy). A colostomy is similar to an ileostomy, but it is made further down the digestive tract and functions differently, with more solid output and less chance of complications.
Will it happen to me?
For many people, their bowel function after reversal is similar to before they had a stoma. Meanwhile, others experience manageable changes that do not much affect their quality of life, and they find that they are able to get on with living as they normally would. However, some people experience changes to their bowel function that are a bit trickier to deal with and may require long-term management.
There are few things that affect someone’s chance of a significantly changed bowel function after a bowel operation, although the reasons for these are not always fully understood.
Problems are more likely to be encountered by women compared with men. This is likely because we are made a little differently, and women tend to have a slightly smaller rectum and shorter anal canal compared with men, as well as facing potential changes to the pelvic floor caused by pregnancy.
Among colorectal cancer survivors, bowel function issues are more common in those whose cancer was at the tail end of their bowel, which usually requires the surgeon to remove more of the rectum. Also, if a cancer is low in the rectum, the surgeon will often take away the tissues that surround the rectum. Taking away these extra tissues reduces the risk of the cancer recurring, but it is thought that it may also damage some of the nerves used in bowel function.
Likewise, these issues are more common among those who have undergone radiotherapy as part of their treatment. This is because radiotherapy, which is used to kill cancer cells, will also damage healthy cells in the bowel. This can produce scarring of the bowel or rectum, known as fibrosis. Fibrosis can make the bowel less flexible and less able move in the same way as it did before, and this may result in bowel symptoms.
Seeking treatment
If you have persistent bowel problems after stoma reversal, you need to tell your surgeon or nurse about your symptoms. They will be able to direct you to the most appropriate of the many potential treatments that might help, or they might ask you to see a specialist nurse who can assist you.
The first treatments to be tried include changes to medication, diet and/or exercise habits. If these do not work, there is most likely an effective solution out there, and there are other, more involved treatment options that can be tried. These options may include transanal irrigation, where a special device is used to empty the bowel with water. This process provides reliable and complete evacuation, letting you then go about your day in safety and confidence.
After stoma reversal, whether or not any issues are immediately evident, you need to be careful when wiping the skin on your bottom with tissues. The skin will not be used to being wiped after your time with your stoma, when you were not using your bowels in the normal way. For the first couple of weeks, while your bowels adjust, it can be worth using barrier cream on this skin to prevent it from getting sore.
Seeking treatment
If you have persistent bowel problems after stoma reversal, you need to tell your surgeon or nurse about your symptoms. They will be able to direct you to the most appropriate of the many potential treatments that might help, or they might ask you to see a specialist nurse who can assist you.
The first treatments to be tried include changes to medication, diet and/or exercise habits. If these do not work, there is most likely an effective solution out there, and there are other, more involved treatment options that can be tried. These options may include transanal irrigation, where a special device is used to empty the bowel with water. This process provides reliable and complete evacuation, letting you then go about your day in safety and confidence.
After stoma reversal, whether or not any issues are immediately evident, you need to be careful when wiping the skin on your bottom with tissues. The skin will not be used to being wiped after your time with your stoma, when you were not using your bowels in the normal way. For the first couple of weeks, while your bowels adjust, it can be worth using barrier cream on this skin to prevent it from getting sore.
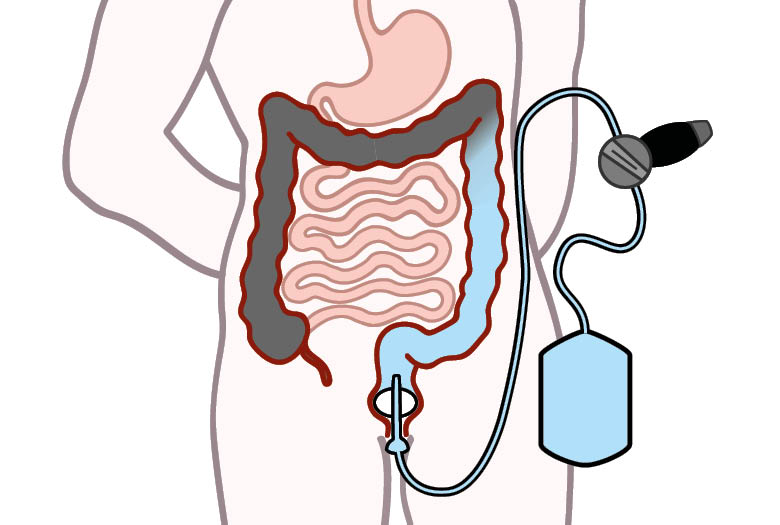
Transanal irrigation
Speaking up
Stoma reversal is usually a welcome event, but it can lead to issues with bowel function. It is important to remember that there are many potential treatments available for these problems, and there is no need to suffer in silence. If you speak about your concerns with an appropriate health professional, such as a specialist cancer nurse, they will be able to guide you.
Jennie Burch is the Head of Gastrointestinal Nurse Education at St Mark’s Hospital, London

